By Shannon Pacella, DPT, PHRC Lexington
The pelvic floor is a phrase used very frequently here on the blog as well as in our clinics, but to those unfamiliar with this area of the body, it may still be this illusive mystery. I want to break down the pelvic floor into each of the muscles it is comprised of, in order for you to get a better grasp of what’s going on down there.
If you are partial to 3D visuals and videos, you can Take a Tour of the Pelvic Floor.
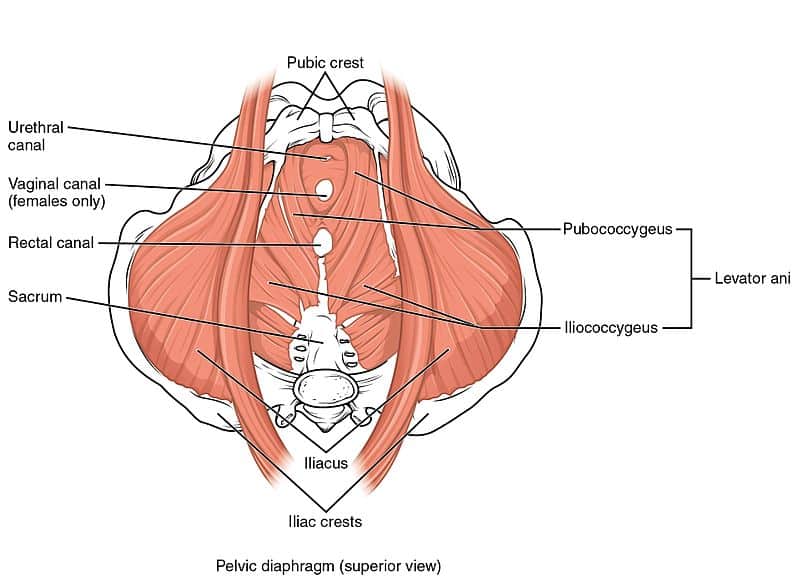
The pelvic floor is comprised of multiple layers of muscles that close off the bony frame of the pelvic outlet and are key in supporting the pelvic organs. To quote from our previous blog post: A Cock in the Hen House: A look inside the Male Anatomy, “Although the external anatomy is different, all the other internal muscles that make up the pelvic floor are the same for men and women. The muscles sit in the pelvis like a muscular bowl, providing support to the organs of the pelvis and assisting in bowel, bladder, and sexual function. In women, the pelvic floor supports the uterus, the bladder, and the colon. In men, the pelvic floor supports the prostate as well as the bladder and the colon.”
First let’s discuss the bones that make up the pelvis/pelvic girdle. The pelvic girdle is a basin-shaped ring of bones connecting the vertebral column to your femurs. The pelvic girdle contains and protects the pelvic organs and allows for attachment of the pelvic floor muscles.
The pelvic girdle is comprised of:
- Ilium: the largest pelvic bones – when you put your hands on your hips you are touching the ilium.
- Ischium: the part of the pelvis that you sit on (aka sit bones).
- Pubis: the front part of the pelvis that joins both sides together via the pubic symphysis.
- Sacrum: the sacrum attaches to the ilium via the sacroiliac (SI) joint.
- Coccyx: also known as the tailbone, and attaches to the lower part of the sacrum.
Now that you have some reference material, let’s go through each muscle one by one:
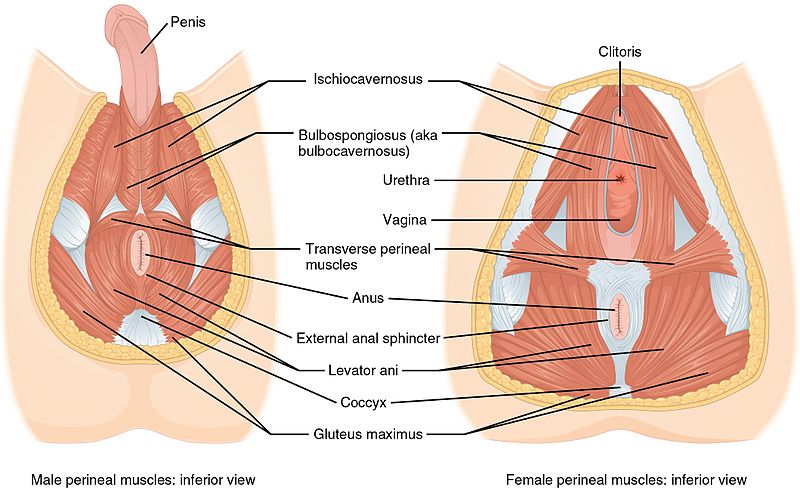
- Bulbospongiosus: in men, this muscle runs along the underside of the base of the penis and forces blood into the penis during erection, and aids in ejaculation. In women, this muscle runs from the clitoris to the perineum along each side, constricts the vagina, and forces blood into the clitoris.
- Ischiocavernosus: attaches from the pubic symphysis to the ischial spine on each side, and forces blood into the penis and clitoris during erection.
- Superficial & Deep Transverse Perineal: this muscle has superficial (thinner band) and deep (broad) fibers that run underneath the perineum – the space between the anus and vagina (in women) or base of penis (in men). Supports the prostate and vagina.
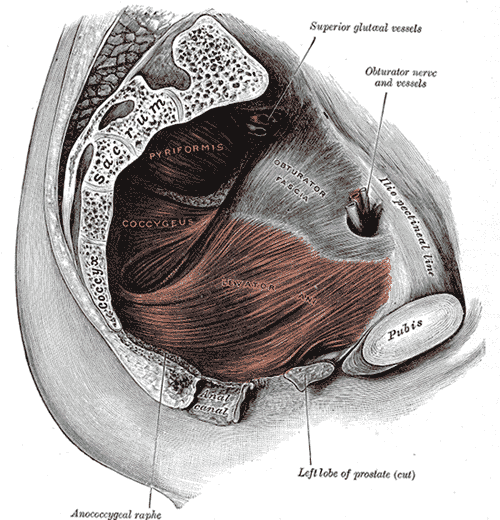
- Ischiococcygeus (aka Coccygeus): attaches from the tendinous arc of the ischial spine to the lower sacrum and coccyx. Moves the coccyx forward and supports the pelvic viscera.
- Levator Ani is a group of muscles (highlighted above in red) comprised of:
- Pubococcygeus: attaches from the pubis to the lower sacrum and coccyx.
- Iliococcygeus: connects with pubococcygeus muscle and attaches to the coccyx.
- Puborectalis: wraps around the rectum to form a muscular sling.
- External Anal Sphincter: attaches to the tip of the coccyx and surrounds the anal canal. This muscle closes the anal orifice.
- Obturator Internus: attaches from the pubis and ischium to the femur, helps to turn your hip outward (lateral/external rotation). *Fun fact: tightness and/or trigger points in this muscle can refer pain to the coccyx/tailbone.
- Piriformis: muscle deep in the buttocks (underneath gluteals), attaches from the sacrum to the femur, also works to rotate the hip outward (lateral/external rotation). Tightness in this muscle can be linked to sciatica (nerve pain down the back of the thigh), due to its proximity to the sciatic nerve.
Whew! That was a lot of information to get through! Now that you have a better understanding of what the pelvic floor looks like, let’s go over some ways this complex area of the body may lead to pelvic floor dysfunction in men and women.
Pelvic Pain
- Vaginal/penile/scrotal/perineal or anal pain
- Tailbone/sacroiliac joint/pubic symphysis pain
- Pain that interferes with sitting and exercise
- Pain that radiates to the abdomen/buttocks/thighs
Urinary Dysfunction
- Urinary urgency, frequency, and hesitancy
- Urinary retention
- Pelvic organ prolapse & incontinence
- Decreased force of urinary stream
- Pain/straining with urination
Bowel Dysfunction
- Constipation
- Fecal Incontinence
- Pain/straining with bowel movements
Sexual Dysfunction
- Pain with intercourse/penetration
- Pain post ejaculaton
I hope this helped to give you a better understanding of the pelvic floor anatomy.
References:
- Carriere B, Feldt CM. The pelvic floor. Germany: Georg Thieme Verlag; 2006.
- Netter FH. Atlas of human anatomy. 6th ed. Philadelphia, PA: Elsevier Inc.; 2014.



Comments
Thank you Shannon,
Your knowledge is so very helpful. I find these articles very informative and interesting.
Great article. Thank you.
I am a 78 y/o male
I have pain confined to the area of my left ischial tuberosity. It is experienced while sitting and relieved by walking or standing. It causes me to stand for long periods and there is collateral damage causing my feet and ankles to become sore and weak.
I had a pelvic PT for 6 months with the therapist identifying the problem as Levator ani syndrome primarily involving the obturator internus muscle. I also had trigger point injections and a steroid anesthetic injection.
I notice that there is not much discussion on ischial tuberosity pain or possibly ischial bursitis disease.
Would appreciate if you could help. This is a very serious life changing experience for me.
Author Shannon Pacella says:
Hi Burt,
I am sorry to hear that you have been dealing with pain for quite some time. Ischial bursitis aka weaver’s bottom, is defined as inflammation of the bursa that separate the gluteus maximus muscle and the ischial tuberosity. It is typically caused by prolonged sitting on hard surfaces. Ischial bursitis occurring on it’s own (without any other pathology) is rare. Typically ischial bursitis is caused by a secondary pathology (which it sounds like may be levator ani syndrome primarily involving the obturator internus muscle as per your pelvic PT).
I would suggest continuing with pelvic floor physical therapy in order to address your functional limitations and help to manage your pain.
I am 59-year-old female who has had several surgeries per what they thought was Vuvodynia!in 1993 they did an Argon Lazer of the vulva cost 3rd degree burns of that area then did a vuvectomy which left me and no better circumstances still so much pain I wanted to die! I had terrible burning of the fall the urethra that was constant and a 10 on the pain scale! They then did many flash pump dies surgeries and grafting to fix the damage that the vulvectomy caused! Still in so much pain they then separate a nerve to that area the peroneal area. With no improvement in pain I then was given an implanted pain infusion Pump which I still have. A few years ago they found I had six Tarlov cyst in the sacral area of my spine a doctor in Kansas City the cysts were in the S1 to S3 Area of my spine and had rounded part of my tailbone any nerves for being constricted by thesis some with nerves running through them ! That was in 2011 and I am still in terrible terrible of our and urethral me with the frequency of urination and can barely sit! This is something I would never wish on my worst enemy and I wish I could get some help for the pain the doctor was Dr. Frank Feigenbaum ! He said it was one of the worst cases he ever seen as far as compression of nerves in the sacral area of the spine. All I want is enough pain relief to be able to live life I have left without suffering every minute of the day!if you have any advice for me I would love to hear it thank you so much for listening!
Author Shannon Pacella says:
Hi Monette,
Thank you for sharing your experience, and the long journey you have endured. Tarlov cysts can be very painful and complex to treat, you can learn more from one of our blog posts: https://pelvicpainrehab.com/pelvic-pain/4561/pelvic-pain-tarlov-cyst/
I suggest being evaluated by a physical therapist who can help direct a treatment plan to improve your quality of life and functioning by reducing and managing your pain and symptoms. Physical therapy is not going to change the cyst itself, but it can lessen some of the symptoms caused by a Tarlov cyst.
Hi, Shannon Pacella. Thanks for sharing this useful information regarding dysfunction. You explained all the dysfunction in an easy and understandable way.
What’s up everyone, it’s my first visit at this web site,
and article is truly fruitful in support of me, keep up
posting such articles or reviews.
Hi Shannon,
Thanks for the information. I am currently seeing a PF PT to address a hip injury from 9 years ago that is now impacting my pelvic floor. My symptoms ( pain in back, SI joint pain and pain down legs -sciatic like) worsen with each monthly period. I dont have a history of endometriosis. Is it possible that PFD can increase sciatic like pain that I’m experiencing? I’m hoping this goes away as I progress with Pelvic PT.
Thank you